Much of what lawmakers on the Senate Health, Hospitals and Human Services Committee heard Tuesday was dire and unsurprising.
Leadership from the V.I. Human Services Department, the Government Hospital and Health Facilities Corporation Board and territory hospitals all testified to the impact of “boarders” — people who were initially admitted for medical reasons and treated, but who cannot take care of themselves and lack the social support needed to be safely discharged.
When referring to boarders in the territory and the lack of long-term care options, testifiers liberally used the word “crisis.”
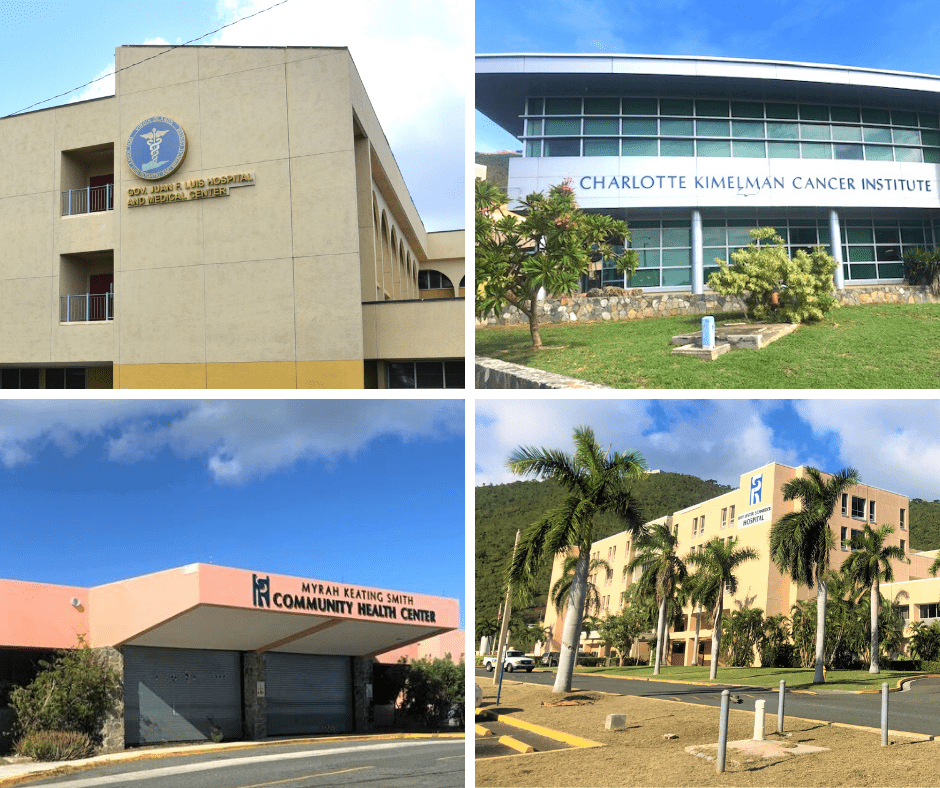
Chief executive officers from both major hospitals testified to insufficient funding in the face of tens of millions of dollars worth of uncompensated care and upticks in money owed to vendors. Schneider Hospital CEO Tina Comissiong put SRMC’s accounts payable at $38 million. Darlene Baptiste, the newly-installed chief executive officer of Luis Hospital, said JFL owes vendors $19.9 million — up $2.2 million since the end of the 2024 fiscal year — after years of paying down arrears.
Human Services Commissioner Averil George said the number of Virgin Islanders enrolled in Medicaid had decreased by more than 13.5 percent since January 2024 — a decrease largely attributed to the sunsetting of Public Health Emergency provisions implemented during COVID-19. At the pandemic’s height, there were 38,489. George said the decrease “raises concerns about individuals losing coverage, highlighting the urgent need for improved outreach, streamlined eligibility processing, and continued federal support to ensure continuity of care.”
The issues testifiers raised aren’t new.

Through no fault of their own, boarders around the country consistently take up beds, lengthen emergency department wait times and overtax hospitals’ already-precarious finances. Rural hospitals are chronically understaffed and underfunded, and during last summer’s budget hearings territory health care providers were clear-eyed about the impact of losing nearly 17,000 Medicaid enrollees.
George said 21,071 Virgin Islanders were enrolled in Medicaid at the end of the last calendar year.
In the 50 United States and the District of Columbia, the federal government matches Medicaid expenditures at a “federal matching assistance percentage” rate — or FMAP — based on the state’s per capita income, according to the federal government’s Medicaid website. For the U.S. Virgin Islands, the federal government now pays 87 percent of costs and the remainder is paid by the territory — but there’s a cap.
Once costs exceed the federal cap, the territory pays for all.
Bryan’s Push for More Funding
Gov. Albert Bryan Jr. has repeatedly named lifting the Medicaid cap among his federal policy goals. As recently as December, a Government House press release described him as visiting the nation’s capital to advocate for “the extension of the rum cover-over excise tax … and the lifting of the Medicaid cap to ensure more equitable healthcare funding for Virgin Islanders” with the outgoing Biden administration and incoming Trump administration.
Bryan was in Washington, D.C. again in the last week, but the Medicaid cap went unmentioned in a Government House video message posted to social media Monday in which Bryan described his meetings with federal policymakers. That’s likely because House Republicans managed to pass a budget resolution late Tuesday extending $4.5 trillion in tax cuts and cutting $2 trillion in government spending. The resolution charges the House Energy and Commerce Committee — which oversees spending on Medicaid and Medicare — with trimming $880 billion in expenditures.
Even if Medicaid funding wasn’t on the chopping block, the dearth of long-term care facilities and services continues to put the territory’s health care institutions in a difficult situation.
Christopher Finch, former chair and current secretary of the Government Hospitals and Health Facilities Corporation Board, said during Tuesday’s hearing that the hospitals cannot bill third-party payers like Medicaid, Medicare or private insurance companies for boarders, who have no medical reason to remain hospitalized. The number of boarders in the territory’s hospitals differed slightly across testimonies, but Finch said boarders occupy nearly half of the general adult beds at JFL North and almost a third at Schneider.
“When we have large numbers of boarders — like now — occupying a significant number of our beds, this results in patients remaining in emergency room beds while they wait for an open bed within the hospital,” he said. “That limits the spaces to see other emergency room patients and is one of the causes of increased wait times.”
Tragic Incidents Raise Questions
Both hospitals’ emergency departments have been home to tragic incidents in 2025.
On Tuesday, lawmakers heard from Edgar Baker Phillips, who reported his sister, 70-year-old Doris Phillips, missing in late January. Phillips said he visited Schneider and was told by staff at the hospital’s front desk that she wasn’t there.
“Since I was unable to locate my sister, I decided to file a missing persons report with the department of Public Safety,” he said. “A Silver Alert was sent out by Public Safety — while she was in the morgue.”
The next day, Phillips said he was told that his sister had been taken by ambulance to Schneider’s emergency department two weeks prior. After making several calls, Phillips learned that his sister had been brought to the emergency department on Jan. 9, where she died from a bleed.
“According to the physician, they were unable to contact individuals who was listed as next of kin,” he said. “The individual who they reported that they contacted said she never received a call from the hospital.”
Phillips said it wasn’t the first time his sister, who had been diagnosed with schizophrenia, was hospitalized at Schneider.
“And they could have looked back … and determined who was the next of kin then, or they could have filed a report with Public Safety,” he said. “Additionally, I went and picked my sister’s belongings up. Her bag had numerous pieces of identification.”
On St. Croix, 41-year-old Samuel Ruiz Jr. was taken by ambulance to Luis Hospital on Jan. 2. According to a V.I. Police Department notice issued that week, he was admitted shortly after noon but was gone by the time his name was called approximately six hours later. According to VIPD, the hospital’s law enforcement officer reported that a nurse found the man behind the generator room the next morning. He was declared dead at 7:30 a.m.
A spokesperson for the V.I. Justice Department told the Source an autopsy performed in January determined that Ruiz died of natural causes. Ruiz’s sister filed a civil complaint in V.I. Superior Court to subpoena the man’s medical records.
A New Way Forward?
Testifiers Tuesday offered a number of ways to improve health care in the U.S. Virgin Islands.
Comissiong, whose hospital weathered two cyberattacks in 2024, spoke to the need for an updated electronic medical records system that would interface with the territory’s health information exchange. Finch testified that the issue of boarders could be alleviated in the short term by giving more money to the Human Services Department to either place people in facilities abroad or expand space in St. Croix’s Herbert Grigg and Queen Louise facilities, once the latter is renovated. Dr. Jerry Smith, the newly seated GHHFC chair, spoke to the need for a territory-wide approach to overseeing U.S. Virgin Islands hospitals.
“Long gone are the days where the two district hospital boards individually ran each of the hospitals and the territorial board met quarterly in a bitter clash,” he said during prepared testimony, adding that the absence of quorums on district boards forced the territorial board to function as a single policy and oversight entity. “I call for the abolishment of the district board and the idea of a territorial board in name and function — and the birth of a cohesive health care system with a centrally-guided ecosystem for its leadership.”
Sen. Hubert Frederick, vice chair of the Senate Health Committee, noted that talks about consolidation could open “Pandora’s Box” but signaled openness to the idea.
“Our cost of operation is high. If you look at the purchasing price for medication, for supplies — everything is so high, but we don’t get a discount, because guess what? We purchase separately,” he said. “What was the board thinking back then, what are they thinking now? Why keep this system that’s failing both hospitals?”
Other lawmakers were more cautious.
“I’ve been around here long enough to know that haste make waste,” said Sen. Novelle Francis Jr., who chairs the Senate Finance Committee. “I think that there needs to be a well thought out plan and there needs to be a feasibility study and determination to ensure how we move forward. I’m very open-minded to this merger — consolidation, if you want to call it that — I totally agree that when you look at economy of scale, we have to look at how we begin to do things differently.”